Understanding Prostate Cancer
Prostate Cancer & Treatment Options
Which cancer treatment should I choose?
“On top of the shock of being diagnosed with cancer, the array of possible treatment plans can leave patients feeling very confused as to which is most appropriate for them.
Some patients feel surprised at being offered a choice of treatments and naturally feel inadequately prepared to make such an important decision.
It is not unusual to require time to consider options or second opinions from other specialists before coming to a decision.”
— Assoc Prof Daniel Moon
Diagnosis and assessment of prostate cancer
A/Prof Moon has been involved in a number of trials testing new methods to find and evaluate prostate cancer:
Some examples are below:
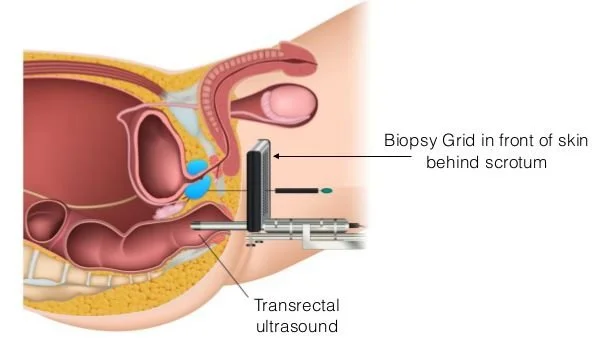
Transperineal prostate biopsy
Multiparametric prostate MRI
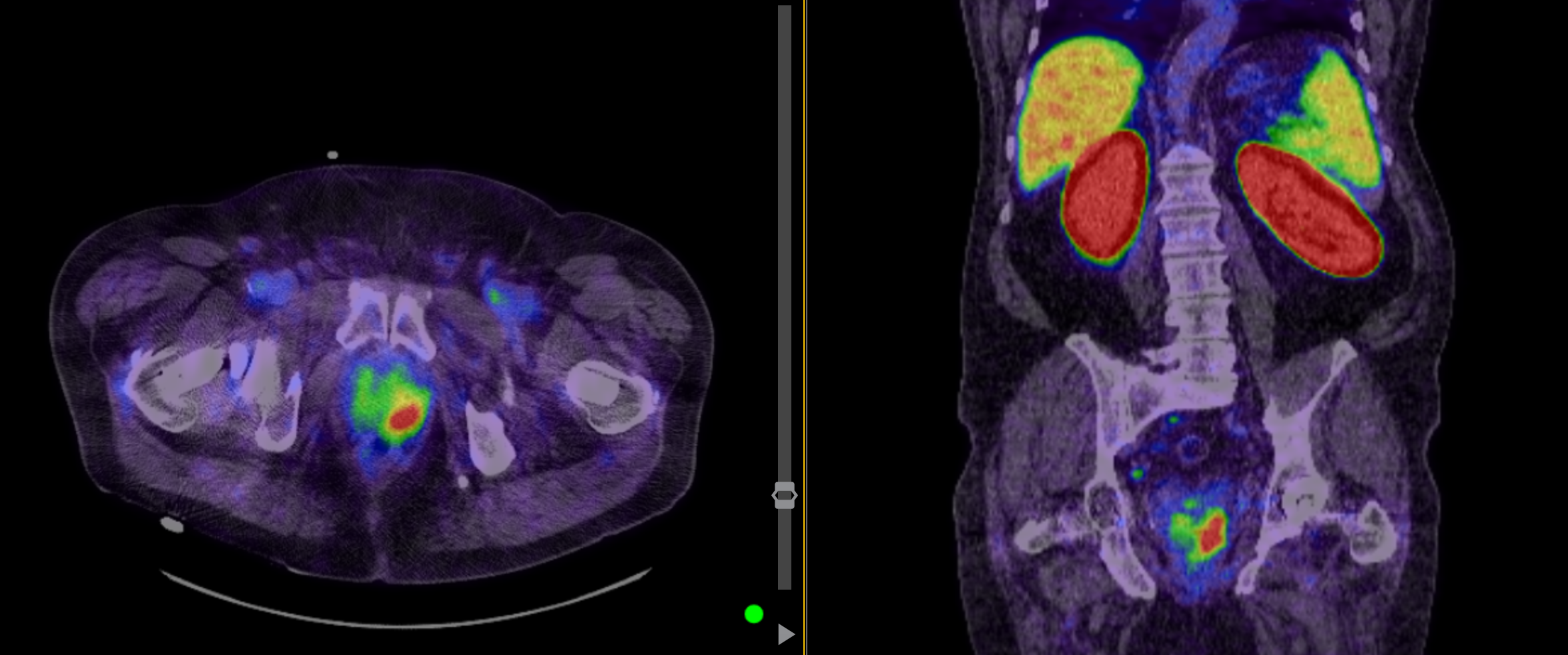
PSMA PET scan
Treatment Options
It’s your decision, seek professional advice and make an informed choice.
There are many ways to treat cancer that is still confined to the prostate (T1 or T2) and there often remains no definite agreement as to which is the best.
One of the reasons for this is that patients with early-stage disease may live 10 years or more if no treatment is used, whereas in others the disease can be more serious and progress quickly. While we can generalize, it is impossible to predict with certainty for any one individual the course their particular cancer may take.
The first thing to note is that you should not feel pressured to make a decision. When prostate cancer is detected early, there is plenty of time to explore your options, and it is not uncommon for patients to take a few months to decide which treatment they would prefer.
-
If only a small amount of slow growing (low grade) prostate cancer is found, a ‘wait and see’ policy may be chosen to assess if the cancer is growing quickly enough to warrant treatment. This is because multiple studies have now demonstrated that low grade prostate cancer will not spread or lead to death.
This does not mean doing nothing but involves a series of tests to decide what threat the cancer poses, and to monitor this carefully over time. If there are signs the cancer is growing or becoming more aggressive (higher grade) then curative treatment can be undertaken.
Tests used to monitor the prostate include:
• PSA testing, including:
o Age adjusted PSA levels
o PSA velocity – how quickly it is rising
o PSA density – adjusting for the prostate size
• Prostate MRI
• PSMA PET scanning
• Repeat prostate biopsy
If treatment is ultimately required, it may be in the form of curative treatment (such as surgery or radiotherapy), or control with hormonal therapy (particularly in the elderly or those with other medical conditions posing a more serious threat)
-
Radical prostatectomy historically was performed as an open procedure, most often through a cut between the belly button and pubic bone.
From 2000, keyhole approaches to this operation were developed, called laparoscopic radical prostatectomy. This approach offered advantages include a better view of the operation for the surgeon, less blood loss, a shorter hospital stay and a quicker recovery.
A further advancement in key-hole surgery was the development of a robotic system that enhances the visualization and precision of the procedure. The first robotic surgical procedure was performed in Australia in 2003. This system replicates the surgeon’s hand movements with instruments that articulate in all dimensions and eliminate tremor, with a full 3D image of the anatomy.
Robotic surgery has steadily replaced open surgery in a number of areas, particularly in prostate cancer surgery, where a meticulous technique is required to preserve the fine and fragile structures involved in bladder control and erectile function. It has been proven in the only randomised trial comparing open and robotic surgery to offer a safer procedure with lower risk of complications. Robotics does require subspecialised training however, and the best results are seen in centres or surgeons performing a high volume of procedures.
-
Radiotherapy is the delivery of radiation beams at the prostate, aiming to destroy the cancerous cells, with minimal impact on surrounding normal structures (bladder, urethra and rectum). It can also be used in a palliative setting, directed at areas of cancer outside the prostate, eg for relief of bone pain due to cancer spread.
Radiotherapy can be administered like an X-ray, by directing the beam from outside the body onto the prostate (external beam radiotherapy), or by inserting radioactive ‘seeds’ or needles into the prostate (brachytherapy). Following radiotherapy, the PSA slowly declines and is monitored to assess the success of treatment, although this can take up to 12-18 months.
-
While most prostate cancer is “multifocal” – occurring in multiple parts of the prostate at the same time, some men have prostate cancer in just one area of the prostate. This can be confirmed through systematic biopies, along with imaging of the prostate using MRI and PSMA-PET scanning. In these men it may be possible to treat just this area of the prostate using techniques such as:
- Nanoknife – uses electrical currents to treat the tumour
- High Intensity Focused Ultrasound (HIFU)
- Focal brachytherapy
Advantages of this form of treatment include avoiding side effects of treating the whole prostate through surgery or radical radiation therapy, and still having the option of radical prostatectomy if the cancer grows back. Disadvantages include the need for closer monitoring after treatment including repeat biopsies to assess treatment success, the higher risk of recurrence, and the lack of long term outcome data, as this form of treatment is relatively new.
-
This treatment is usually offered to patients in whom the cancer has spread beyond the prostate, eg to lymph glands or bone. Prostate cancer is partly driven by the male hormone, testosterone, which is made by the testicles. By stopping the production of testosterone, the cancer usually significantly shrinks in size throughout the body, and is held dormant for a period of time that may last many years. Ways to achieve this consist of either:
surgically removing the testicles (orchidectomy) taking medications, or
3-6 monthly injections to ‘turn off’ the testicles.
The effectiveness of treatment can be monitored by the PSA reading, which quickly drops in most patients.
Side effects are those of a loss of the male hormone and are similar to the menopause experienced by women as they lose their female hormones.
These may consist of fatigue, loss of libido, loss of erections, hot flushes, tender or enlarged breasts, loss of muscle bulk.
Over time the bones may lose strength (osteoporosis) with increased risk of fracture, and therefore it is recommended to have regular bone density scans.
Hormonal therapy is not a cure, as with time the cancer begins to grow again despite the treatment, but is an effective control that in some patients can last for a long period of time.
What are your surgeon’s results?
“This is the question that all men should ask their surgeon when considering treatment options.
— Assoc Prof Daniel Moon
In addition to Dr Daniel Moon’s presented and published outcomes, he also contributes to the Prostate Cancer Outcomes Registry of Australia and New Zealand, which can compare prostate cancer surgeons’ caseload and results.
The Prostate Cancer Outcomes Registry has been independently collecting outcomes of men treated for prostate cancer since 2009.
Over 10000 cases of prostate cancer have now been collected and the analysis is ongoing.
Through quarterly reports outcomes can be reported by surgeons for :
positive margin rates ie has the cancer been completely removed? This is a marker of the quality of surgery performed, and should be kept as low as possible.
Urinary bother suffered by men at 12 and 24 months post-operatively
Sexual bother suffered by men at 12 and 24 months post-operatively
Get in touch:
03 9967 0198
-
Call us on 03 9967 0198 or use our contact form to send us your details. We will get in touch to arrange your initial consultation appointment.
When making a booking, please let our friendly staff know if you would prefer an in-person or telehealth appointment.
-
We are conveniently located opposite Cabrini Hospital Malvern at 198 Wattletree Road, Malvern with parking on site.
Also consulting at:
134 Bay st, Brighton with parking on site
Telehealth consultations available upon request
Please arrive 10 minutes before your scheduled appointment time as there can be some documentation to attend to before your appointment.